Medical billing process step-by-step provides a vital glimpse into the complex world of healthcare finance, where every detail counts and precision is paramount. Navigating this intricate system can seem overwhelming, but understanding the sequence of events can make it far less daunting. Whether you’re a healthcare provider, a patient, or someone simply interested in the workings of medical billing, this guide will unravel the layers and highlight the essential components involved in this process.
From the initial patient encounter to the final payment, each phase of the medical billing process plays a crucial role in ensuring that healthcare providers are compensated for their services. By breaking down the steps methodically and providing clarity on the necessary documentation, this overview aims to demystify the billing journey and underscore the importance of accurate coding and diligent follow-up.
Overview of the Medical Billing Process

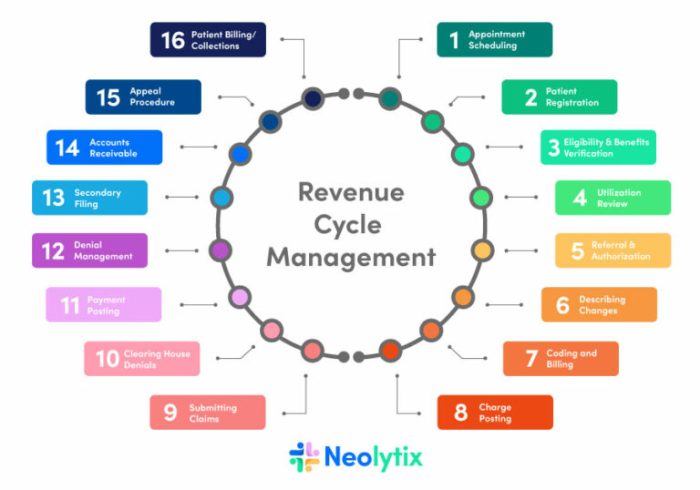
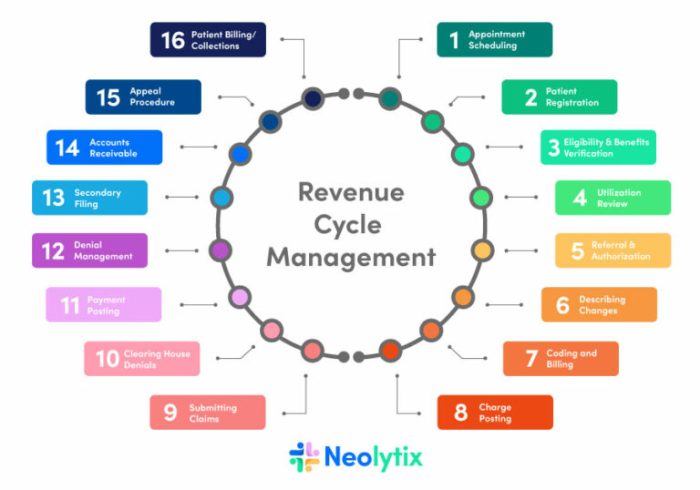
The medical billing process is a crucial aspect of the healthcare system, playing a pivotal role in ensuring that healthcare providers are compensated for their services. This process not only involves the submission of claims to insurance companies but also encompasses various steps that ensure accuracy and compliance with regulations.The significance of medical billing lies in its ability to streamline the revenue cycle, minimize errors, and enhance cash flow for healthcare providers.
A well-organized billing process ensures that patients receive the care they need without unnecessary financial burdens. Additionally, it helps maintain a transparent relationship between providers, patients, and payers.
Key Components Involved in Medical Billing
Understanding the components of the medical billing process is essential for healthcare professionals and billing specialists. Each part of the process contributes to the overall efficiency and effectiveness of billing operations. Below are the key components involved in medical billing:
- Patient Registration: This initial step involves gathering essential patient information and verifying insurance details. Accurate data collection here can significantly reduce claim denials later.
- Charge Entry: This involves documenting the services provided to the patient in a detailed manner. Each service corresponds to specific codes that are necessary for billing.
- Claim Submission: Once charges are documented, claims are submitted to the appropriate insurance payers. This step requires adherence to coding guidelines and regulations to avoid errors.
- Payment Posting: After claims are processed, payments received from insurance companies are recorded. This helps in tracking the revenue cycle effectively.
- Accounts Receivable Follow-Up: This ongoing process involves monitoring outstanding claims and following up on unpaid or denied claims to ensure timely payments.
A visual representation of the medical billing process can be illustrated as follows:
Step 1
Patient Registration A patient visits a healthcare provider, providing personal and insurance information.
-
Step 2
Charge Entry
- The healthcare provider records services rendered, which are then translated into specific billing codes.
- The coded information is submitted to the insurance company for reimbursement.
- The insurance company reviews the claim, decides on the payment, and sends an explanation of benefits (EOB).
- Payments are received and recorded into the provider’s billing system.
- Any discrepancies, denials, or outstanding payments are addressed and resolved.
Step 3
Claim Submission
Step 4
Insurance Processing
Step 5
Payment Posting
Step 6
Follow-Up
Effective management of these components is vital for maximizing revenue and maintaining the financial health of healthcare practices.
Step-by-Step Breakdown of Medical Billing
The medical billing process is a crucial component of healthcare operations, ensuring that providers are compensated for their services. Understanding the sequential steps involved can enhance efficiency and reduce errors in billing practices. This breakdown will guide you through the essential stages of medical billing, highlighting necessary documentation and the role of medical coders in maintaining accuracy.
Initial Patient Visit and Information Collection
The medical billing process begins when a patient visits a healthcare provider. Accurate data collection is essential at this stage to ensure smooth billing later on. Key documents required include:
- Patient registration form: This form gathers personal information, including demographics and insurance details.
- Insurance card: A copy of the patient’s insurance card is necessary for verification of coverage.
- Medical history: A record of the patient’s previous health issues and treatments helps in providing appropriate care and billing.
Medical Coding
Once the patient has received treatment, the next step involves translating the services provided into standardized codes. This is where medical coders play a pivotal role. They assign codes using ICD (International Classification of Diseases) and CPT (Current Procedural Terminology) coding systems. Accurate coding is critical, as it directly affects billing accuracy and reimbursement rates.
- ICD Codes: These codes represent diagnoses and are essential for identifying the medical necessity of services.
- CPT Codes: These codes correspond to the procedures performed during the patient visit and must accurately reflect the services rendered.
- Modifiers: Modifiers may be used to provide additional details on the service performed, which can influence the payment received.
Accurate coding can reduce claim denials by up to 50%, emphasizing the importance of this step in the billing process.
Claims Submission
After coding, the next step is submitting claims to the insurance company. This process requires careful preparation of the claims to ensure compliance with insurance requirements. The necessary documentation typically includes:
- Superbill: A detailed invoice that includes all services rendered, along with corresponding codes.
- Claim form (CMS-1500 or UB-04): This standardized form is used to submit claims for reimbursement.
- Supporting documentation: Any additional documents that may be required by the insurance provider to process the claim.
Payment Posting
Once claims are processed, the insurance company will issue payment. Payment posting involves recording the payments received and reconciling them against the outstanding balances. Important aspects include:
- Explanation of Benefits (EOB): This document Artikels what services were covered, the payment amount, and patient responsibility.
- Payment entries: Accurate recording of payments received from insurance and patients is essential for financial tracking.
Follow-Up on Denied Claims
Denied claims require prompt attention and follow-up to ensure that providers receive the payments owed to them. This step is crucial in maintaining the financial health of a medical practice.
- Denial codes: Understanding the specific reasons for denial helps in addressing issues effectively.
- Appeal process: Submitting an appeal may be necessary if a claim is denied, requiring additional documentation or clarification.
Best Practices in Medical Billing
Effective medical billing is vital for the financial health of healthcare providers. Implementing best practices can streamline the billing process, reduce errors, and enhance revenue cycle management. This section highlights essential strategies for optimizing medical billing while avoiding common pitfalls.
Common Mistakes in Medical Billing and Avoidance Strategies
Medical billing can be complex, and errors can lead to denied claims and delayed payments. Recognizing frequent mistakes allows healthcare providers to take proactive measures. Here are key errors and strategies to avoid them:
- Inaccurate Patient Information: Incorrect patient data can cause claim denials. Always verify patient demographics and insurance details at each visit.
- Incorrect Coding: Misusing codes can lead to billing issues. Familiarize staff with Current Procedural Terminology (CPT) and International Classification of Diseases (ICD) guidelines.
- Failure to Obtain Pre-Authorizations: Not securing necessary approvals can result in non-payment. Implement a systematic process for tracking authorization requirements.
- Neglecting Timely Claims Submission: Late submissions can lead to lost revenue. Establish a timeline for claim processing to ensure timely submissions.
Importance of Follow-Up and Appeals in the Billing Process
Follow-up and appeals are crucial components of an effective medical billing process. Timely follow-ups ensure that claims are processed and paid, while appeals can recover denied claims. Consistent monitoring of claim statuses allows for rapid resolution of issues. A structured approach to follow-up includes:
- Regularly checking on the status of submitted claims.
- Documenting all communications with payers to create a clear record.
- Timely appeal submissions for denied claims, adhering to payer guidelines.
“A proactive follow-up can turn a denied claim into a collected payment.”
Checklist for Healthcare Providers to Improve Billing Procedures
Creating a checklist can help healthcare providers maintain consistency and accuracy in their billing practices. An organized approach promotes effective billing and minimizes errors. Consider the following checklist elements:
- Verify patient eligibility and benefits before the appointment.
- Ensure accurate coding of diagnoses and procedures.
- Gather and document all necessary patient information.
- Submit claims promptly after services rendered.
- Monitor accounts receivable regularly for outstanding claims.
- Train staff on the latest billing regulations and software tools.
Wrap-Up
In conclusion, grasping the medical billing process step-by-step is essential not just for healthcare professionals but also for patients seeking to understand their healthcare expenses. By recognizing the common pitfalls and the best practices that enhance billing accuracy, stakeholders can ensure a smoother financial transition within the healthcare system. This journey through medical billing not only empowers providers and patients but also fosters a more efficient, transparent healthcare environment.
Popular Questions
What is medical billing?
Medical billing is the process of submitting and following up on claims with health insurance companies to receive payment for healthcare services provided.
Why is medical coding important?
Medical coding is crucial because it translates healthcare services into standardized codes, ensuring accurate billing and compliance with regulations.
How can mistakes in medical billing be avoided?
Common mistakes can be avoided by implementing thorough checks, regular training for billing staff, and using automated billing software.
What role do insurance companies play in medical billing?
Insurance companies review and approve claims submitted by healthcare providers, determining the payment amounts based on coverage policies.
What should I do if my medical claim is denied?
If a claim is denied, review the denial reasons, rectify any issues, and submit an appeal if necessary, including proper documentation to support your case.






